PRODUCTS
EZClaim Products
EZClaim is a medical billing and scheduling software company that provides a feature-rich practice management system specifically tailored for the small to medium-sized provider office and outsourced medical billing firms. It also includes integrations with a number of EMR/EHR vendors.
EZClaim’s Medical Billing
Whether you are a doctor, practice manager, or billing service owner, EZClaim Billing is designed with you in mind, simplifying your claims management from data entry to payment posting—and beyond.
EZClaim primarily supports the following specialties: General Practice, Therapy, Vision, Surgical, Medical Specialties, Home Health Care, and Outsourced Medical Billing Services (RCM). However, the software is very adaptable and can be used for many other billing specialties.
EZClaim’s billing software allows the creation of insurance payor lists for Medicare, Medicaid, Tricare, Clearinghouse payer IDs, governmental MCO’s, auto insurance, and worker compensation groups.
EZClaim serves anyone submitting CMS 1500 (professional) or UB-04 (institutional) charges for reimbursement.
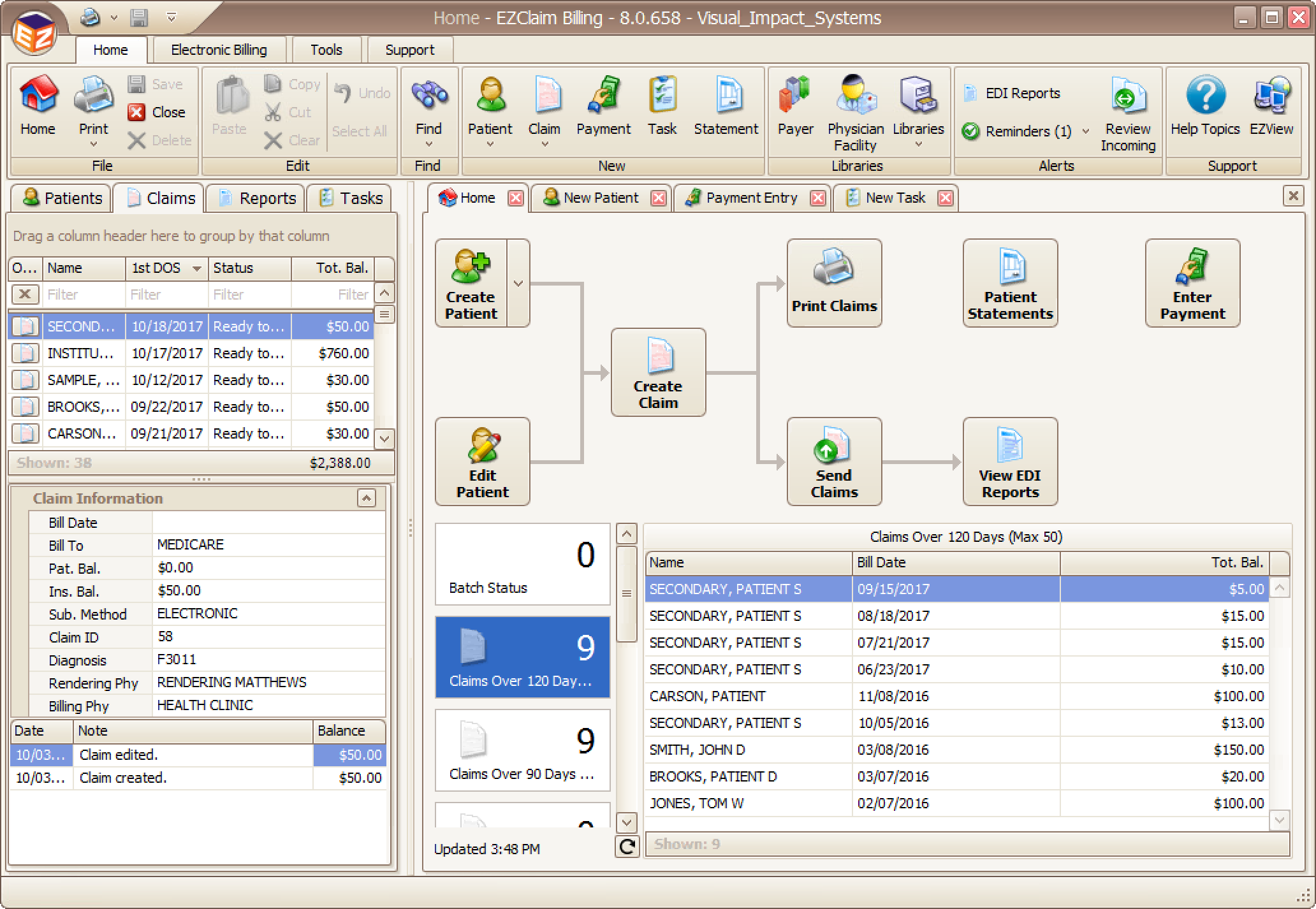
EZClaim Billing Key Features
Whether you are a doctor, practice manager, or billing service owner, EZClaim Billing is designed with you in mind, simplifying your claims management from data entry to payment posting—and beyond.
EZClaim Billing’s Interfaces
EZClaim partners with EHR systems, clearinghouses, statement and payment services, HIPAA compliance, claim scrubbing, MIPS compliance, appointment reminders, and inventory management to provide an integrated, comprehensive solution for your practice.
EZClaim’s numerous interface options help to power this ecosystem of connected tools to streamline your workflow. For more information or questions, contact sales.
[ For more specific details, click either on the category or the company name below. ]
EZClaimPay
EZClaimPay is a new ‘feature’ added to the Billing software. It is EZClaim’s own payment platform to make the Billing software MORE POWERFUL—by making accepting credit and debit cards for payment PAINLESS!
Have ANY Of These Problems?
• Inaccurate Bank Deposits
• Monthly Reconciliation Hassles
• Data Protected on Secure Servers
• Statements are Hard to Understand
• New Fees Showing Up
• Poor Support Experiences
ALL Problems Have Been SOLVED!
• Simplified Payments Reconciliation
• Pricing You Can Understand
• Lower Fees and No Confusion
• Single Source of Support
• Payment Can Be Made Online
• Credit Cards Are Stored Securely on File
EZClaim’s ‘CLOUD’
EZClaim is a “SaaS” (Software as a Service) product. That means that the software ‘resides’ in the ‘Cloud’ (on a server connected to the Internet). One then accesses the Billing and Scheduling applications via the Internet, not on their computer. This frees one from installing and maintaining both the software and the hardware.
This is why EZClaim now is a “subscription” service rather than a “purchase” of a product. The subscription allows a company access to the software “on-demand,” and has many benefits.
Cloud Features
• No Contracts
• Nightly Backups
• Data Protected on Secure Servers
• Program Support and Updates Included
• Works on All Operating Systems
• Less Onsite Technical Support Required
• Dedicated Onboarding Coach Included
EZClaim Billing Software Pricing
EZClaim’s pricing is COST-EFFECTIVE and very simple to understand:
• First (single) user is $159 per month; All additional users are $109 per month*
[ One company file is included for the first (single) user ]
• Additional COMPANY FILES are $30 per month
• PORTALS are $10 per user
Services Included:
• Designated Onboarding Coach or self-serve option
• Training during Onboarding
• Daily backup of cloud data
• Online and live support resources
• Statement customized with your company logo
* NOTE: Additional clearinghouse fees may apply.
Get EZClaim Billing Software Now!
If you are familiar with EZClaim BILLING software and just want to purchase a software license directly, the following self-service purchase form will allow you to do that.
All you need to do is provide the number of Billing Software users, the number of Company Files you will need, and the number of Portal Users you will need.
RCM OPTIONS
EZClaim’s BILLING software is designed to allow outsourced billing and revenue cycle management.
EZClaim’s Scheduling
EZClaim Scheduling integrates with our EZClaim Billing software or can be used as a standalone product.
Create and view patient appointments, convert appointments into claims, collect a payment, populate reports, and simplify your workflow.
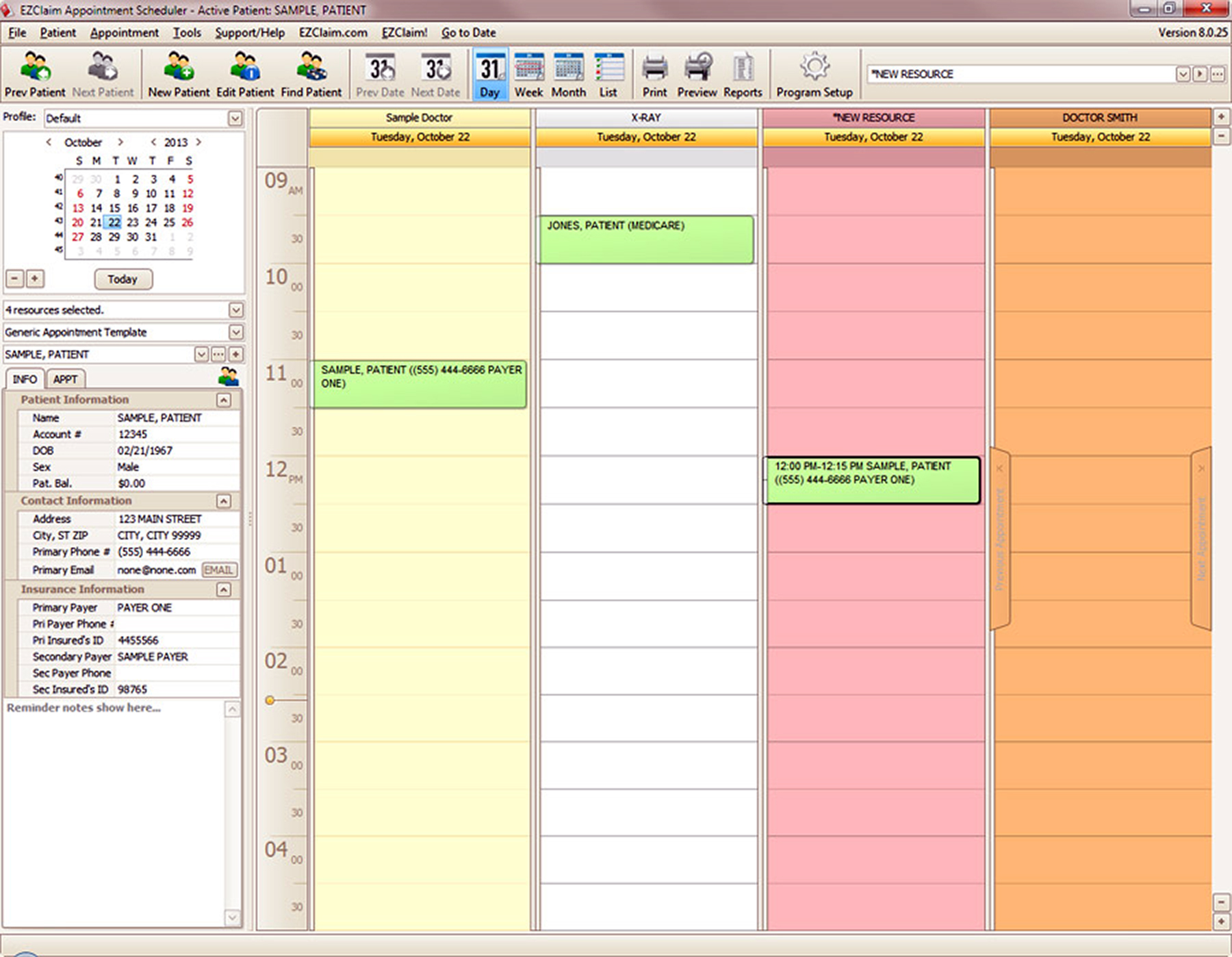
EZClaim Scheduling’s Key Features
Scheduling shares the patient information with EZClaim Billing. Changes made to the patient information in Billing are reflected in Scheduling. In addition to that, changes made in Scheduling are reflected in Billing.
Another benefit of using Scheduling and Billing together is the ability to transfer appointments and generate claims. The transfer function makes use of EZClaim’s claim templates feature. Even though this is not required, claim templates may help in preventing extra data entry once an appointment has been transferred to Billing.
Scheduling Features
• Fully Integrated with EZClaim Billing
• Convert Appointments to Claims
• Drag and Drop Appointment Creation
• Customize Border and Background Colors
• Search for Open Time Slots
• Track Authorized Visits
• Appointment Templates
• Scheduling Alerts
• Eligibility Options
• Record Patient Payments
• Print Patient Receipts
• Customize Super Bill
• Appointment Wait List
• Reminder Notifications with ReminderCall
EZClaim’s PORTAL
The EZClaim Portal is a low-cost option available to anyone using EZClaim Cloud to quickly gain read-only access to their EZClaim data. This Portal helps in reducing delays in communication, giving more visibility to Providers, and helping deliver peace of mind without a large financial commitment.
If you are a billing service with multiple Company Files and would like to allow a Provider access to a single Company File, the EZClaim Portal is for you!

EZClaim Portal’s Key Features
EZClaim’s Portal is HIPAA compliant, is fast and secure, allows 24×7 access, and is cost-effective.
Portal Features
• Access Patients Along with Patient Balances
• Run Reports by Specific Patients
• Control User Access to Widgets and Reports
• Expand or limit user access
• Add or remove users instantly
• Display activity logs at any time
• Brand the Portal with your company logo
Have Any Questions?
EZClaim If you have any questions either, click on the Chat in the lower right corner of this window, call the sales team now at 877.650.0904, or click here to send us an e-mail.

